Health
Effective Management of Multiple Medications
So, you’re taking medications? Welcome to the club! As we age, it’s no surprise that we sometimes find ourselves juggling multiple medications to stay in tiptop shape. But fear not, my fellow seasoned individuals, because today we’re going to dive into the art of managing those pills like a pro. Get ready for some medication magic!
Health is wealth, they say, and taking care of our body requires a little extra effort as we age. A crucial part of this journey is understanding the medications we take and how they interact with one another. After all, we don’t want our daily pill cocktail turning into a merry-go-round that leaves us feeling out of sorts.
Let’s start with the basics. First and foremost, always consult your trusted healthcare provider when adding or changing medications. They’re the experts, and their guidance is gold. Now, let’s get organized!
Make a list
Pen and paper or a nifty smartphone app? It doesn’t matter as long as you have a handy list of all your medications. Include the drug names, dosages, and frequencies. And don’t forget to update it whenever there’s a change.
Color-coding fun
Why settle for a dull list when you can jazz it up? Assign a specific color to each medication and mark the pill bottles accordingly. Not only will it add a fun twist to your routine, but it’ll also make it easier to keep track of what goes into your body.
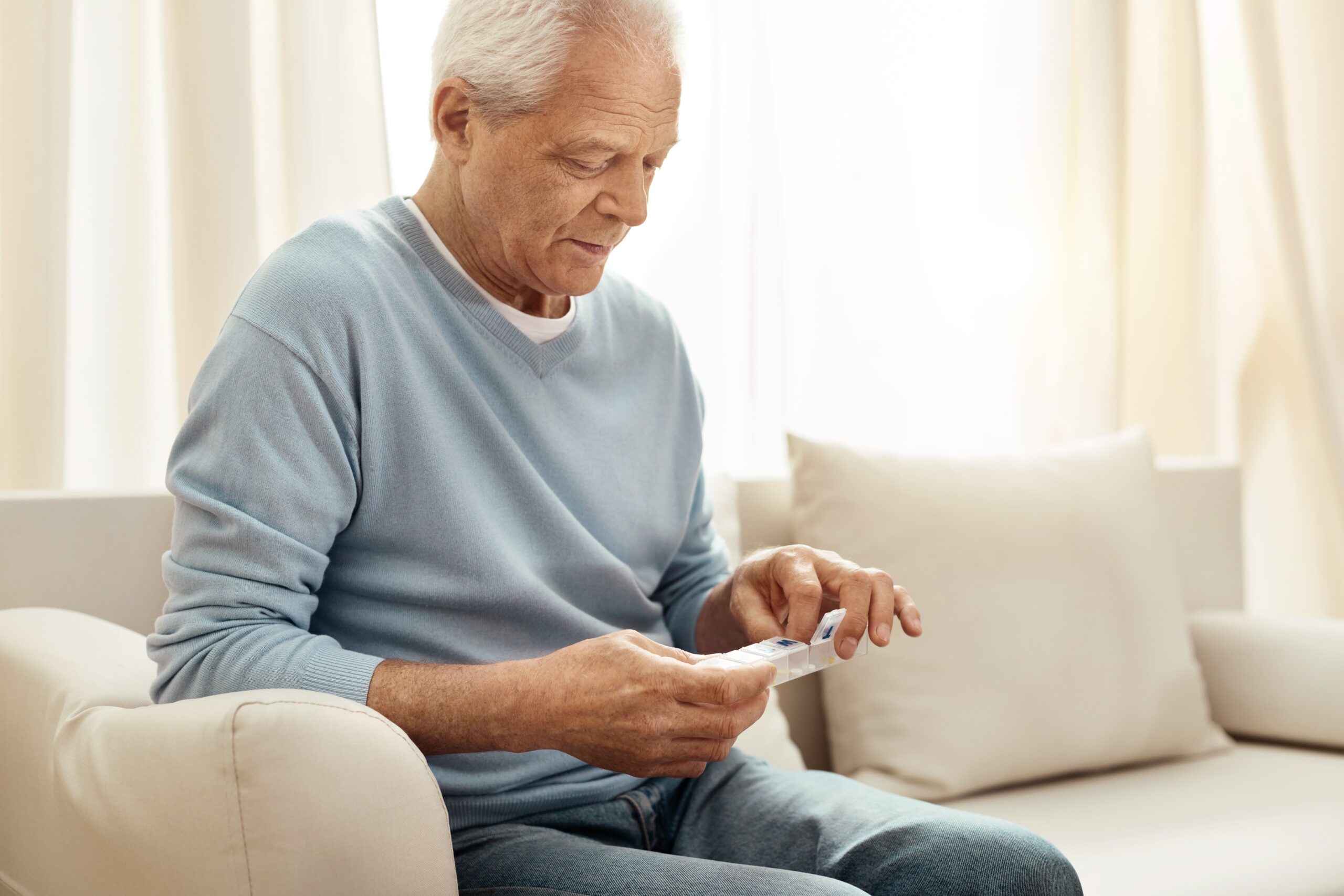
Pill organizers
Get yourself a snazzy pill organizer with compartments for each day of the week. Make it a part of your morning ritual, like having a cup of coffee or doing a crossword puzzle. It’s a little act of self-care that ensures you start the day off right.
Now that we have the organizational aspect covered, let’s look at some tips and tricks to make the whole medication management gig even smoother.
- Timing is everything – Some medications work best when taken on an empty stomach, while others need to be accompanied by food. Read those instruction leaflets like a boss and plan your meals and snacks accordingly.
- Play the name game – Let’s admit it, medications often have these mind-boggling names that make Scrabble masters envious. But fear not! Create catchy nicknames for your medication based on their appearance or purpose. “The little blue one for the heart” or “The round yellow superhero” – you get the drift. It’ll make remembering and discussing them a breeze.
- Dance party reminders – Who says taking medication can’t be a dancing affair? Set a fun alarm tone on your phone that’ll make you want to groove your way to the pill bottle. Dancing optional, but strongly encouraged.
- Side effect bingo – Ah, those lovely side effects! Keep a sense of humor about them by turning them into a game. Create a bingo card with common side effects like drowsiness, dry mouth, or the occasional funky taste, and cross them off as you experience them. Just remember, laughter truly is the best medicine.
- Tea time magic – Depending on the type of medication you’re taking, certain teas can help alleviate side effects or complement their effects. Explore the world of herbal teas and find the perfect match for your health needs. It’s like a cozy retreat for your taste buds.
So, my fellow pill-poppers, embrace your inner medication manager extraordinaire. Remember, a little organization, a touch of creativity, and a dash of humor go a long way in ensuring you stay on top of your health game. And if all else fails, just dance it out, my friend. Cheers to a happy, healthy, and oh-so-balanced life!
Disclaimer: The information provided in this article is for entertainment purposes only and should not replace professional medical advice. Always consult your healthcare provider for personalized guidance.